Background: If we take a look at wikipedia (1), we see that both vegetarians and vegans have lower mortality rates from heart disease, compared to regular meat eaters:
Wikipedia also states that:
In the table we see that occasional meat eaters, vegetarians and fish eaters had similar risks of mortality from all-causes. These were lower than mortality rates from regular meat eaters. However, vegans had mortality rates identical to those from regular meat eaters.
Conclusion: a meta-analysis of 5 prospective studies showed that both vegetarians and vegans had lower mortality rates from heart disease than regular meat eaters. However, in the case of vegans, this did not lead to lower risk of mortality from all causes.
References:
1) Wikipedia. Veganism. Wikipedia page last modified on 26 February 2012. http://en.wikipedia.org/wiki/Veganism
2) Key TJ et al. Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr. 1999 Sep;70(3 Suppl):516S-524S. http://www.ajcn.org/content/70/3/516S.full
A 1999 meta-analysis of five studies comparing vegetarian and non-vegetarian mortality rates in Western countries found that the mortality rate due to ischemic heart disease was 26 percent lower among vegans compared to regular meat eaters, but 34 percent lower among lacto-ovo vegetarians (vegetarians that eat dairy products and eggs) and pescetarians (those that eat fish but no other meat).
Wikipedia also states that:
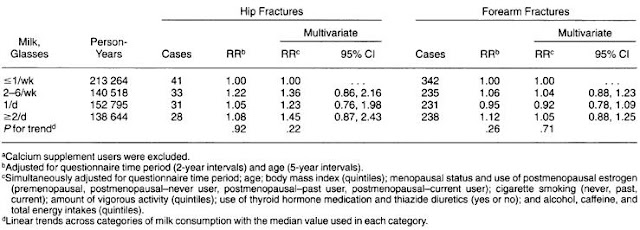
No significant difference in mortality was found from other causes.This line suggests that both vegetarians and vegans may live longer than regular meat eaters. Results from the article referred to (2) can be seen in the following table:
In the table we see that occasional meat eaters, vegetarians and fish eaters had similar risks of mortality from all-causes. These were lower than mortality rates from regular meat eaters. However, vegans had mortality rates identical to those from regular meat eaters.
Conclusion: a meta-analysis of 5 prospective studies showed that both vegetarians and vegans had lower mortality rates from heart disease than regular meat eaters. However, in the case of vegans, this did not lead to lower risk of mortality from all causes.
References:
1) Wikipedia. Veganism. Wikipedia page last modified on 26 February 2012. http://en.wikipedia.org/wiki/Veganism
2) Key TJ et al. Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr. 1999 Sep;70(3 Suppl):516S-524S. http://www.ajcn.org/content/70/3/516S.full






 12:19 PM
12:19 PM